Summary: New research highlights neuroglia ( or glia cells ) as critical players in mental health, potentially influencing conditions like depression and schizophrenia. Glia cells, much considered” help cells” in the mind, have now been shown to speak through special calcium indicating, impacting cerebral function and stress responses. Reports suggest that compromised astrocyte work, a glial body type, does relate to depressive symptoms and schizophrenia.
With the development of new technologies, scientists can create parietal cells from available cells, such as skin, for the purpose of personalized psychiatric care and research. This study aims to change psychiatry from symptom-based to mechanism-based treatment, promising a upcoming of personalized therapies.
Important Information:
- Around 50 % of the cellular structure of the brain is made up of glia cells, which have unique indicating powers that affect mental health.
- In animal experiments, astrocyte function has been linked to depressive-like symptoms, which may affect how people respond to particular antipsychotic drugs.
- New techniques may change a patient’s epidermis cells into parietal cells for personalized investigation, possibly leading to more specific treatments.
Origin: University of Colorado
Only recently have neuroglia, a diverse group of brain cells that support neurons and serve a variety of purposes, been the subject of study. Due to that, head exploration focused strongly on the part of cells.
But as studies continue, experts extremely suspect that these cells, usually called glia tissues or “nerve glue”, does play an important role in medical ailments, such as depression and schizophrenia.
” When we think of the brain we’re usually thinking about neurons, but that’s only about 50 % of what makes up the brain”, says Sukumar Vijayaraghavan, Ph. Dr., who formerly led a facility that looked into the body’s signaling systems and is now a professor of biology and biology at the University of Colorado School of Medicine.
The other cells, neuroglia, were believed to function as the body’s cleansing employees, keeping the environment suitable for maximum cerebral signaling. Then, researchers discovered that neuroglia have a distinct signaling mechanism from the electrical signals that neurons emit. Glia cells have calcium signals.
” We started wondering what all these cells do”, says Vijayaraghavan, who first took up an interest in glia cells more than 20 years ago.
As it turns out, a lot.
Vijayaraghavan is the first author of a recent clinical commentary on this topic , appearing , in , Biological Psychiatry ,.
” Integrating neuroscience into psychiatry”
A subset of neuroglia, called astrocytes, seem to be intricately connected to how the synapses work in neurons, and because these cells play a role in the brain’s stress response, it’s possible that they are connected to some mental health conditions.
” Calcium signaling was the key impetus to this field in the sense that we found that they have elaborate mechanisms of signaling to each other, to the neurons, and to the , blood vessels , in the brain”, Vijayaraghavan says.
” We previously thought they were non-excitable cells, but it’s actually a unique form of excitability”.
In a 2017 , study, researchers in China showed that when astrocyte function is compromised, animal models tended to develop depression-like symptoms. Vijayaraghavan and Andrew Novick, MD, Ph. This is just one example of how glia cells” seem to play a crucial role in psychiatric illness,” according to D., D., assistant professor of psychiatry.
According to the essay,” There are also differences based on the clinical profiles of astrocytes from people with psychiatric disorders as well as from those from healthy control participants.”
” For instance, one study enrolled people who had schizophrenia and had either responded to or failed a clozapine ( an antipsychotic medication ) trial. Both groups ‘ astrocytes had weak glutamate signaling.
” The cool part is what happened next: When they exposed astrocytes to clozapine, glutamate signaling normalized—but only in the group of clinical responders,” they continue.
A better understanding of neuroglia might also be beneficial in clinics.
Many , psychiatric disorders , are primarily described in terms of symptoms. The problem with that, researchers say, is that there may be many reasons for those symptoms.
We’re integrating neuroscience into psychiatry because it thinks more mechanistically about what is actually happening, says Vijayaraghavan.
Technology and the future
Novick stresses the importance of being able to explain to patients what possible brain malfunctions are and why they are experiencing psychiatric symptoms. So far, that can be difficult to do.
” If you went to the doctor with a stomachache and they only responded with a medicine that could fix the stomachache but not what actually caused the stomachache, that would n’t be satisfactory,” Novick says.
” That’s not a proper understanding of things, and so we’re trying to figure out what’s causing these psychiatric diseases, not just how to treat them.”
Fortunately, investigating glial cells may help meet both of those aims.
” From all the data we have, we know that there seems to be a connection between astrocytes and depression,” Novick says.
” This means there’s likely some impact from drugs used to treat depression, and so that’s an important aspect of how understanding these cells influences psychiatry.”
New technology is allowing deeper investigation into , glia cells. A person’s skin or blood cell can now be programmed into an embryonic state and transformed into the cell of interest, which is simpler to obtain than a glial cell.
We discover a lot of astrocytic markers that are linked to conditions like depression. According to Vijayaraghavan, one may wonder whether that will provide us with a diagnostic or even predictive tool to examine what these astrocytes are doing and what causes depression.
In the future, this work could help develop personalized treatments.
” We could take a cell from a person with schizophrenia or depression, make , astrocytes , and figure out the dysfunction and design a therapeutic with the individual in mind,” Vijayaraghavan says.
About this information on neuroscience and mental health
Author: Kara Mason
Source: University of Colorado
Contact: Kara Mason – University of Colorado
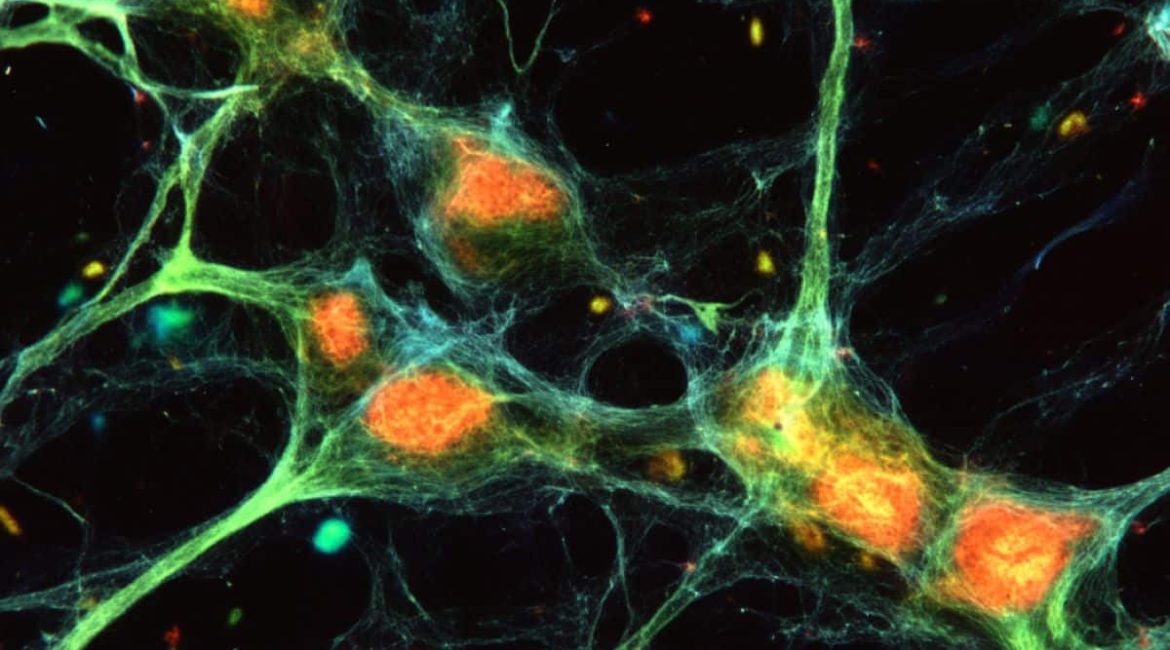
Image: The image is credited to Neuroscience News
Original Research: Open access.
Sukumar Vijayaraghavan and others wrote,” Under the Microscope: Nerve Glue and the Evolution of Psychiatric Neuroscience.” Biological Psychiatry
Abstract
Under the Microscope: Nerve Glue and the Evolution of Psychiatric Neuroscience
In December 1993, at the annual meeting of the American College of Neuropsychopharmacology, psychiatrist David Healy was bored. So, he decided to try something.
He emailed a number of well-known psychiatrists and scientists to ask if they would be interested in talking about their lives and careers.
The stories were amazing: from the discovery of the monoamine system, to the first human trials of reuptake inhibitors, to how antipsychotics evolved from the mysterious chlorpromazine to highly specific D2 , antagonists.
He ultimately compiled these interviews into a 4-volume series entitled , The Psychopharmacologists. In many ways, these stories inform the identity of the modern psychiatrist.