Summary: Researchers have identified how cerebrovascular disease ( CeVD ) disrupts brain connectivity, contributing to cognitive decline and neurodegeneration alongside Alzheimer’s disease ( AD ). They found distinct but antioxidant effects of CeVD and AD-related signs on cognition and brain hypertrophy by studying older adults ‘ head networks and body biomarkers. CeVD acts as a global industry of mental contact networks, while Advertising markers, such as blood p-tau181, follow distinct pathways.
These findings highlight the potential for combining heart biomarkers and neuroscience to detect and monitor dementia earlier. The study provides fresh insights into the distinct roles that CeVD and AD play in influencing architectural and cognitive mind changes. Future studies aims to improve mental communication markers in order to support earlier forecasts and targeted interventions.
Important Information:
- Dual Pathways: While never synergizing, CeVD and AD markers freely and additively impact cognition and brain deterioration.
- Mental Connectivity Impact: CeVD disrupts world mind network communication, influencing mental decline.
- Forecast Biomarkers: Neuroimaging and blood-based signs show promises for first dementia risk assessments.
Origin: NUS
Researchers have gained novel insights into how Alzheimer’s disease ( AD ) pathology and cerebrovascular disease ( CeVD ) dysfunctions in older adults interact with brain function disruptions to affect neurodegeneration and cognition.
The research team, led by Associate Professor Juan Helen Zhou, Director of the Center for Translational Magnetic Resonance Research at Yong Loo Lin School of Medicine, National University of Singapore ( NUS Medicine ), discovered a brain functional connectome phenotype that is linked to several CeVD markers and contributes in any way to cognitive decline and neurodegeneration along with AD.
CeVD is a worldwide industry of brain connectivity, which is changing how we understand its role in dementia.
CeVD, usually co-occurring with Advertising, has long been a major area of study in age and dementia research. It refers to a number of conditions that have an impact on the blood vessels and blood flow in the brain, including stroke, cerebral atherosclerosis ( narrowing or hardening larger brain arteries as a result of plaque buildup ), and small vessel disease that affects the tiny blood vessels in the brain.
By preventing the supply of oxygen and nutrients, which are necessary for normal mental function, these conditions can cause brain damage.
In the study, published in , Alzheimer’s &, Dementia: The Journal of the Alzheimer’s Association, the team  , examined the body’s functional entity in 529 older adult individuals across the memory variety, ranging from those with good thinking to individuals diagnosed with AD.
The team looked at the relationship between the various signs of CEVD and brain activity habits, and how each of the respondents ‘ responses to each other’s brain activity habits was influenced by a global functional international, or a distinctive pattern in the brain’s communication channel, that is strongly linked to the presence of four different markers of CEVD, which are seen on brain scans.
A key finding of the study was the identification of divergent effects of , p-tau181, a blood-based biomarker for AD, and CeVD-related functional connectome phenotype on cognitive decline and brain atrophy.
The study found no evidence of a synergistic relationship between CeVD and , p-tau181, which suggests that these two factors may have an impact on neurodegeneration in distinct pathways, despite the two contributing additively to longitudinal cognitive decline and brain atrophy.
A/Prof Zhou said,” We discovered that a CeVD-related brain network phenotype, along with a key Alzheimer’s disease blood biomarker, can provide powerful insights into the future trajectory of cognitive decline and neurodegeneration.
Our findings “underline the importance of integrating neuroimaging and blood biomarkers to better understand the pathophysiology of these co-occurring diseases” and “highlight the potential of brain connectome-based markers to track cognitive decline, particularly for those at-risk for dementia.
Dr. Joanna Su Xian Chong, senior research fellow from A/Prof Zhou’s group and the study’s first author, continued,” This pattern shows how the burden of multiple cerebrovascular disease markers can collectively have a significant impact on brain function.
” Importantly, the combination of this pattern linked to CeVD and plasma , p-tau181, a marker of Alzheimer’s disease, had independent and additive effects on long-term outcomes.
” Together, they contributed to cognitive decline and increased brain atrophy at baseline and over time, but did not interact directly to amplify each other’s effects.”
Both A/Prof Zhou and Dr. Chong are graduates of NUS Medicine’s Human Potential Translational Research Programs, as well as the Center for Sleep and Cognition and Healthy Longevity.
The team’s goal is to find out how the severity, cause, and location of CeVD markers affect the brain communication pattern throughout the disease’s progression.
Additionally, they intend to look into how this pattern and various AD markers interact to cause brain decline and degeneration in various cognitive domains. Additionally, they want to know whether these brain network characteristics can be used as a reliable biomarker to track the progression of cognitive decline, particularly in those who are degenerative.
These characteristics could aid in the early identification of long-term cognitive outcomes and provide more accurate predictions than conventional brain imaging techniques.
Their goal is to develop advanced imaging tools for early detection and disease monitoring to better understand the brain mechanisms underlying CeVD and AD.
Funding: This research is supported by the National Research Foundation, Singapore under the NMRC Open Fund – Large Collaborative Grant ( MOH-000500 ) and administered by the Singapore Ministry of Health through the NMRC Office, MOH Holdings Pte Ltd.  ,
The National University Hospital and St. Luke’s Hospital recruited as study participants.
About this news about neuroscience research
Author: Gladys Sim
Source: NUS
Contact: Gladys Sim – NUS
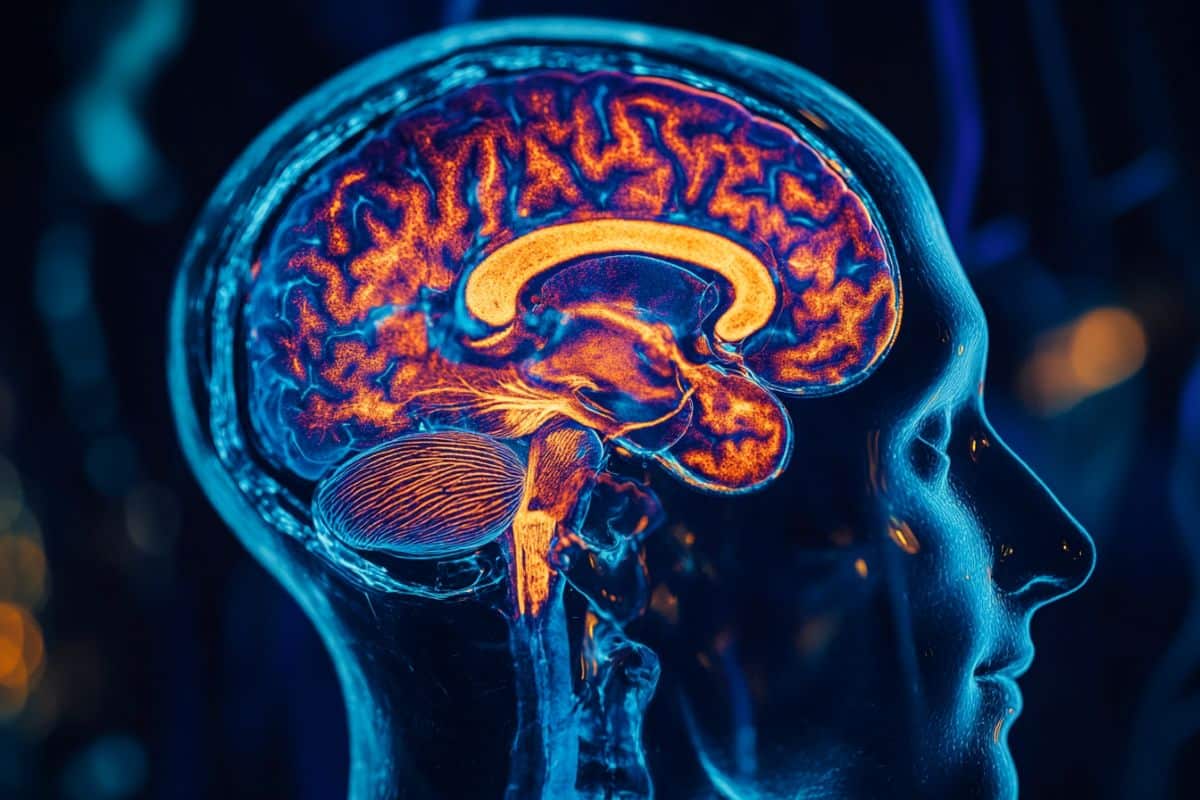
Image: The image is credited to Neuroscience News
Original Research: Open access.
Juan Helen et al.,” Functional connectome phenotype and plasma p-tau181 have additive effects on cognitive outcomes and longitudinal neurodegeneration.” Alzheimer’s &, Dementia
Abstract
Functional connectome phenotype and plasma p-tau181 have additive effects on cognitive outcomes and longitudinal neurodegeneration.
INTRODUCTION
We investigated the effects of multiple cerebrovascular disease ( CeVD ) neuroimaging markers on brain functional connectivity (FC), and how such CeVD-related FC changes interact with plasma phosphorylated tau (p-tau ) 181 ( an Alzheimer’s disease]AD] marker ) to influence downstream neurodegeneration and cognitive changes.
METHODS
Plot least squares correlation was used to examine the associations between five CeVD markers, whole-brain FC, and five dementia-related multivariate associations in 529 participants. Using linear mixed-effects models, the interactivity of CeVD-related FC patterns and p-tau181 on longitudinal gray matter volume ( GMV) and cognitive changes was investigated.
RESULTS
We found a brain FC phenotype with a high CeVD burden across all markers. Further, expression of this general CeVD-related FC phenotype and p-tau181 contributed additively, but not synergistically, to baseline and longitudinal GMV and cognitive changes.
DISCUSSION
Our findings highlight the significant impact of AD and CEVD on neurodegeneration and cognition, suggesting that CeVD has global effects on the brain connectome.