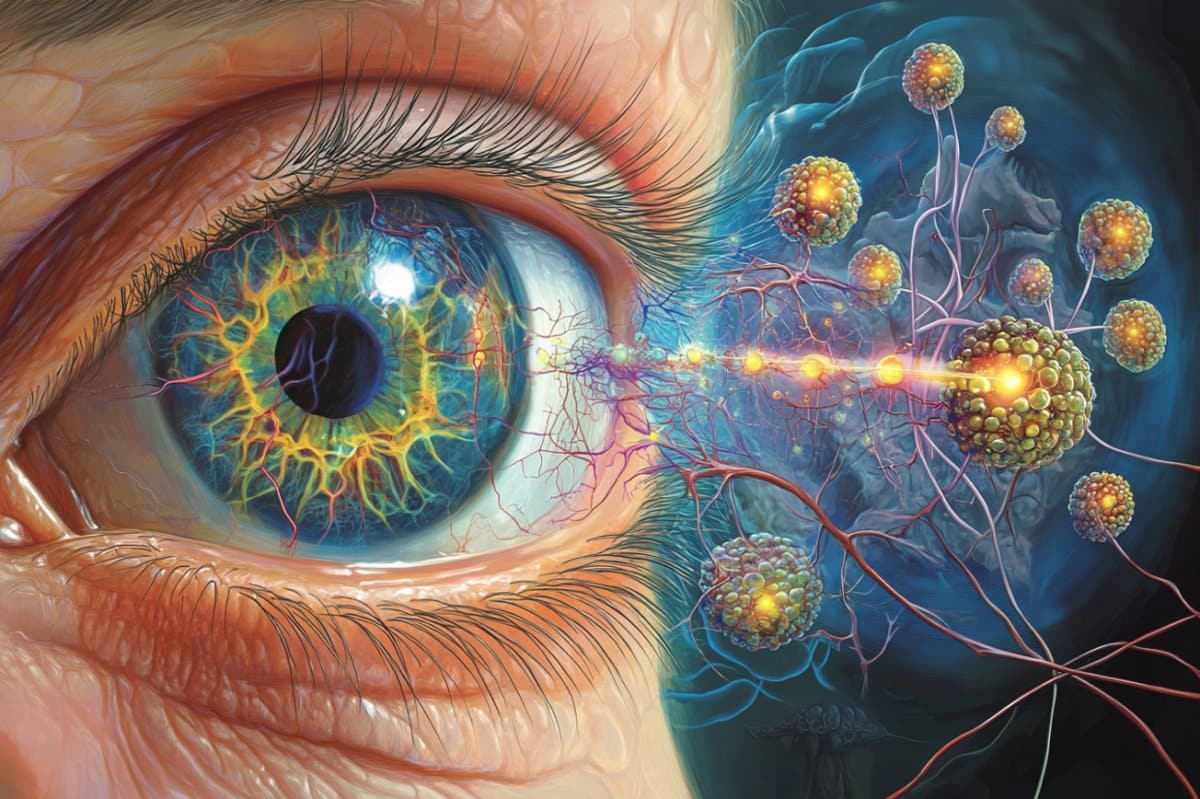
Summary: Age-related macular degeneration ( AMD), the leading cause of adult blindness, affects nearly half of people over age 80. New research is uncovering how retinal cells communicate using microRNA and extracellular vesicles ( EVs ), with the goal of slowing AMD progression.
Researchers found that when microRNA-204 fails to regulate fat digestion in ocular defensive cells, inflammation accelerates degradation. The group hopes to scientist EVs to provide medical cargo to microglia, probably rejuvenating aging cells and providing a more efficient alternative to existing AMD treatments.
Important Information:
- MicroRNA Malfunction: Loss of microRNA-204 functionality in ocular microglia may cause AMD.
- Vehicles as Therapy: External particles had been engineered to provide treatments to defense cells in the retina.
- Recent Solutions Lag: Existing doses for AMD just help 10–15 % of patients, highlighting the need for new methods.
Origin: University of Oklahoma
It’s an unfortunate fact of aging: Life much enough and, finally, reading this word will get tough, also impossible.
Three in 10 Americans older than 80 have some form of age-related macular degeneration ( AMD), while for Oklahoman octogenarians, it ’s closer to 50 %.
Nowadays, new research from the University of Oklahoma aims to highlight the causes of AMD and support professionals stare into a black box of blindness.
With help from a four-year,$ 1. 7 million award from the National Institutes of Health , Jiyang Cai, Ph. D. , a professor of biology and physiology at the OU College of Medicine, is studying how cells in the retina talk and whether the emails they send could be programmed to behave or delayed AMD, the leading cause of adult myopia.
Cai and associates believe one cause for AMD occurs when a little protein, called microRNA-204, is no longer able to message the protein that regulates fat in ocular microglia tissues, which help maintain immune work in the eye.
“ When we see more lipids in the microglia, we know that something is wrong, ” Cai said. “It means that the microglia aren’t doing their job. ”
To determine how the breakdown occurs, Cai and colleagues are mapping the links between cells and genes in the eyes of laboratory mice.
Age-related macular degeneration begins with weakening of retinal pigment epithelium cells ( RPEs ), a layer of cells that support the retina’s photoreceptors. When degeneration occurs, the affected tissues call in immune cells to clear the metabolic products, which in turn triggers chronic inflammation.
In published and preliminary studies, Cai has determined that RPE cells send signals via miRNA to microglia by using extracellular vesicles ( EVs ), tiny delivery vans that transport packages of information.
The research team also found that microRNA-204 targets the Tgfbr2 gene in microglia, which is involved in inflammation and fat metabolism.
They are now trying to understand is whether extracellular vesicles from RPE cells can be used or engineered to rejuvenate aging retinal microglia. In other words, perhaps the delivery vans can be programmed to carry cargo that is beneficial to the retina.
“We want to figure out how microRNAs in these extracellular vesicles interact inside the microglial cells, which might provide a mechanism for future treatments, ” Cai said.
“ Until now, we’ve just watched something get fed into a black box and done a readout of what comes out, ” he said.
“With this research, we’re trying to understand how cargo contents within EVs might contribute to the therapeutic effects of these vesicles. ”
Cai said the results of these studies will provide insights into how EVs and their associated cargoes interact with two distinct cell types in the outer retina.
The findings could also guide future applications of EV-based delivery of compounds to modulate microglia function and alleviate the progression of age-related retinal diseases.
If successful, the strategy would be a welcome departure from current therapies. For patients with dry macular degeneration, the most common form of the disease, treatment includes injecting antibodies directly into the eye.
Unfortunately, these treatments are only about 10-15 % effective at slowing the progression of the disease, Cai said. There are currently no treatment options for many of the patients with late-stage AMD.
Still, as promising as the work is, Cai said it won’t turn back time. Weaker vision is simply a part of getting older.
“We’re looking to slow the progression of the degeneration rather than preventing it from happening, ” he said. “Everybody will get some kind of degeneration with aging. But maybe we can turn it into a minor annoyance rather than a life-changing eventuality. ”
About the Project
Funding: The research reported in this news release is supported by the National Eye Institute, a component of the National Institutes of Health, under award number R01EY035855-01A1.
The content of this news rlease is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
About this AMD and visual neuroscience research news
Author: April Wilkerson
Source: University of Oklahoma
Contact: April Wilkerson – University of Oklahoma
Image: The image is credited to Neuroscience News