Summary: A recent study examined neurons affected by PTSD at the single-cell levels, examining various genetic variations that might contribute to the problem. Researchers studied adult body nuclei to compare contact differences between PTSD, major depression, and power brains, and focused on the dorsolateral prefrontal cortex, a brain region responsible for mental regulation.
They discovered opposing designs of microglial action in PTSD and depression, and affected signaling in antagonistic neurons in PTSD, which might account for hyperarousal symptoms. Vascular endothelial cells in PTSD brains even displayed symptoms of difficulties, possibly resulting in more anxiety hormone coverage.
Important Information
- PTSD neurons showed decreased communication from antagonistic neurons, which may be the cause of hyperexcitable, overreactive mental states.
- Endothelial cells in Sad brains were physically altered, affecting the access to stress hormones, and microglia were active in melancholy but underactive in PTSD.
- New Therapeutic Pathways: The investigation identified gene channels that could be blasted with PTSD-specific, especially developed, detail medicines.
Origin: Yale
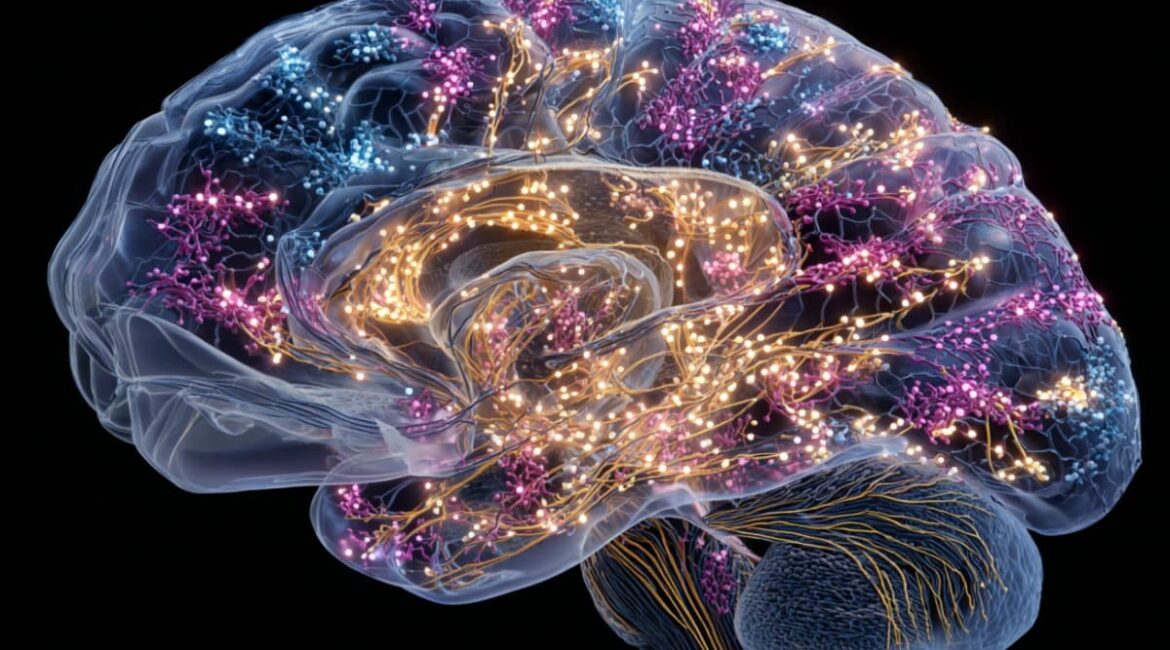
Millions of connected organisms that are constantly talking to one another make up the human mind.
A brand-new study from Nature studies the single-cell level to examine how this cellular communication may be malfunctioning in brains affected by post-traumatic stress disorder ( PTSD ).
Scientists were unable to study genetic variant within adult cells until recently.
A team led by Matthew Girgenti, PhD, assistant professor of psychiatry at Yale School of Medicine, has been studying brain cells to find genetic variants that might be linked to psychiatric disorders like major depressive disorder ( MDD ) and PTSD.
Their most recent research is one of the first to look at a significant medical condition, PTSD, at the single-cell level.
Because there are no medications specifically designed for PTSD, specialists have been prescribing drugs for decades to treat the condition.
Girgenti hopes that discovering fascinating chemical patterns linked to the medical condition will aid researchers in developing new drugs or repurposing already used ones to handle it more efficiently.
In order to understand the physiological methods that are in play in these conditions, he says,” We’re trying to figure out what’s gone wrong in medical problems.”
The final goal is to find areas where we can possibly treat them, as the saying goes.
For the new study, the analysts used postmortem people brain cells from both PTSD sufferers and sponsors.
To better understand both the commonalities and where chemical differences between the conditions, they also examined tissues from people who had been diagnosed with MDD, which is frequently diagnosed in people with PTSD.
They exclusively examined the dorsolateral prefrontal cortex, a part of the brain responsible for administrative functioning and psychological regulation.
Girgenti explains that this area of the brain is” the most distinctively people.”
The researchers studied individual cells from each of the three groups, paying particular attention to the cells, which package the cell ‘ DNA and produce RNA. The team was able to watch genetic variation between the parties as a result.
Important chromosome changes were discovered in MDD and PTSD patients.
The evaluations revealed gene modifications in a type of nerve known as antagonistic neurons in brains with PTSD.
Girgenti claims that these cells are” the fine tuning neurons.”
They manage the various cells and stop them from overfiring.
The amount of interaction between these cells decreased in hippocampus with PTSD and MDD, according to the team’s findings. The researchers think that this sluggish contact may be a cerebral cortex hyperexcitable state.
Following a traumatic event, hyperexcitability may lead to symptoms that are typically associated with PTSD, such as hyperarousal ( overreactive fight-or-flight response ) and nightmares.
Additionally, the researchers found disparities in the immune cells known as microglia in the brain. They found, surprisingly, that these tissues were communicating more effectively in neurons with MDD than in those with PTSD.
According to Girgenti, “PTSD and MDD are typically very similar to one another and have a lot of shared hereditary variability.”
” This getting seems to distinguish between the two,” the author writes. His team wants to look into these differences more and how they might affect the two conditions.
Additionally, they discovered that implicated endothelial cells also had genomic alterations in PTSD brains. These tissues communicate with the rest of the system and are a part of the body’s arteries. Prior research has demonstrated that PTSD sufferers have higher levels of stress hormone that travel through blood vessels to the head.
Because these epithelial cells are compromised,” we think there may be an increase in the amount of stress hormone that enters the brain,” says Girgenti.
unlocking brain strategies to help us develop innovative treatments
Scientists are very little aware of the physiological mechanisms underlying PTSD, in contrast to Alzheimer’s disease and Parkinson’s condition, which are associated with discernible changes in the brain when seen. By going deeper into the chemical realm, Girgenti hopes that these discoveries will help create more effective treatments for the condition.
We’ve now identified pathways that we believe are targetable by certain medications, he claims. Pathways refer to how genes communicate with one another.
” These particular tissues and those personal chemical changes alone made this possible,” he continued. We must then try to find medications that can correct that.
Girgenti’s team intends to look into different brain regions that might be involved in PTSD disease, such as the brain, which regulates the production of stress hormones.
Girgenti notes that” the dorsolateral prefrontal cortex has been thoroughly studied.”
However, there are other brain areas that we don’t know much about, and they’re really as likely to hold techniques for what’s wrong. And there are potential perhaps better therapeutic areas to consider.
The Department of Veterans Affairs, the Brain and Behavior Research Foundation, the American Foundation for Suicide Prevention, the State of Connecticut’s Department of Mental Health and Addiction Services, the National Institutes of Health ( awards R01AA031047 ), DP1DA060811, R01NS128523, and R01HG012572 ) as well as Yale University supported the research that was cited in this news article.
The writers are only responsible for the content, which does not necessarily reflect the National Institutes of Health’s official position.
About this information from science and Anxiety
Author: Isabella Backman
Source: Yale
Contact: Isabella Backman – Yale
Image: The image is credited to Neuroscience News
Start access to original research.
The human brain’s single-cell transcriptional and protein dynamics are implicated in PTSD, according to Matthew Girgenti and al. Character
Abstract
In PTSD, the human brain’s single-cell transcriptional and protein dynamics are implicated.
Post-traumatic stress disorder ( PTSD ) is a genetic disorder that results from prolonged stress exposure. Recent reports have begun to examine the molecular science of PTSD.
However, it is improbable that a single body type is to blame for the variety of PTSD-perturbed chemical pathways identified thus far, given the array of them.
We present a report of the chemical responses in more than two million cells from the dorsal frontal cortex of 111 people brains, which were taken from both PTSD and major depressive disorder.
We map the epigenomic regulome of PTSD in a cell-type-specific way and discover cerebral and non-neuronal cell-type regions, protein expression changes, and regulatory authorities.
Our research identified PTSD-associated dna alterations in microglia, endothelial cells, and antagonistic neurons, as well as genes and pathways linked to glucocorticoid signaling, GABAergic transmission, and neuroinflammation.
We used cell-type-specific spatial transcriptomics to more validate these studies, which revealed the disruption of important genes like FKBP5 and SST.
In a cell-type-specific context, we integrated hereditary, transcriptomic, and genomic data to discover the regulation mechanisms of reputable variants that disrupt PTSD genes, including ELFN1, ELFN1, MAD1L1, and KCNIP4 in a gene expression-specific context.
Together, these findings provide a thorough analysis of the cell-specific chemical regulatory systems that control the cerebral cortex’s persistent effects from the traumatic stress response.