Summary: A recent study has found that Alzheimer’s patients and newborn babies both have elevated levels of the exact proteins, p-tau217, in their body. Although this peptide is a crucial component of Alzheimer’s, it appears to support healthy brain development and growth in children.
First infants had the highest levels, and they steadily dropped after birth, suggesting that earlier brain wiring played a part. Understanding how young children safely manage these large tau levels may lead to the development of new methods to treat or prevent Alzheimer’s.
Important Information:
- Shared Biomarker: Both Alzheimer’s and children have high levels of the p-tau217 in their body.
- Various Procedures: In infants, elevated p-tau217 supports mind development, unlike in Alzheimer’s, where it signals disease.
- Medical Cases: Understanding a child’s ability to adapt to tau does inform upcoming Alzheimer’s treatments.
University of Gothenburg, cause
What do the neurons of young children and those who have Alzheimer’s disease have in common?
Researchers from the University of Gothenburg, under the direction of first author Fernando Gonzalez-Ortiz and senior author Kaj Blennow, recently discovered that both children and Alzheimer’s people had elevated levels of a protein called activated tau, especially a form known as p-tau217.
Although this protein has primarily been used as an Alzheimer’s disease diagnostic test, it is thought that an increase in p-tau217 bloodstream levels is caused by a different process, especially the aggregation of b-amyloid protein into amyloid plaques.
Interestingly, in children, increased plasma p-tau217 seems to reflect a totally different – and fully healthy – mechanism. Children do not have this type of compulsive change ( for natural causes ).
Researchers analyzed blood samples from more than 400 people, including good children, premature babies, young people, older adults, and people with Alzheimer’s disease, in a big international study that included Sweden, Spain, and Australia.
The highest levels of p-tau217 were found in newborns, which was even higher than those found in those with Alzheimer’s. These levels were particularly high in premature infants, and they gradually decreased over the first few months of life before settling down to adult levels.
First time in newborns ‘ blood
Previous studies had suggested that phosphorylated tau might play a role in early brain development, largely based on animal models. For the first time in human newborns ‘ blood, scientists have directly measured p-tau217 levels, giving us a much more comprehensive understanding of its developmental role.
Here’s where it becomes fascinating, as p-tau217 in Alzheimer’s disease is linked to tau aggregation into dangerous tangles, which are thought to cause the breakdown of brain cells and subsequent cognitive decline.
In contrast, this rise in tau in young people appears to promote healthy brain development, allowing neurons to grow and establish new connections with other neurons, and shaping the young brain’s structure.
Additionally, the study found that p-tau217 levels were closely related to how early a baby was born in both healthy and premature babies. The higher the levels of this protein, which suggests a role in facilitating rapid brain development in challenging developmental conditions, the earlier the birth.
Potential roadmap for new therapies
The most intriguing aspect of these findings, which were published in the journal Brain Communications, is the suggestion that our brains may have once had built-in defense against the harmful effects of tau, so that newborns can tolerate, and even benefit from, high levels of phosphorylated tau without triggering the kinds of damage seen in Alzheimer’s.
” We think that understanding how this natural protection functions and why we lose it as we get older could provide a roadmap for new treatments. We might one day mimic those processes to slow or stop Alzheimer’s in its tracks if we can learn how the newborn brain manages tau, says Fernando Gonzalez-Ortiz.
Therefore, a rise in p-tau217 levels is a risk signal in older brains, but in new ones it might be a crucial component of developing one. The same molecule, playing two radically different roles, one building the brain and the other indicating its decline.
The FDA has recently approved the use of plasma p-tau217 to diagnose Alzheimer’s disease, making it a crucial tool in clinical settings.
The authors stress the importance of fully understanding the mechanism responsible for the rise in p-tau217, especially when interpreting it as a result in clinical and epidemiological research and in drug development.
This study suggests that p-tau217 increases may not be the main cause of these increases.
About this news about neurodevelopment, Alzheimer’s disease, and genetics.
Author: Margareta G. Kubista
Source: University of Gothenburg
Contact: Margareta G. Kubista – University of Gothenburg
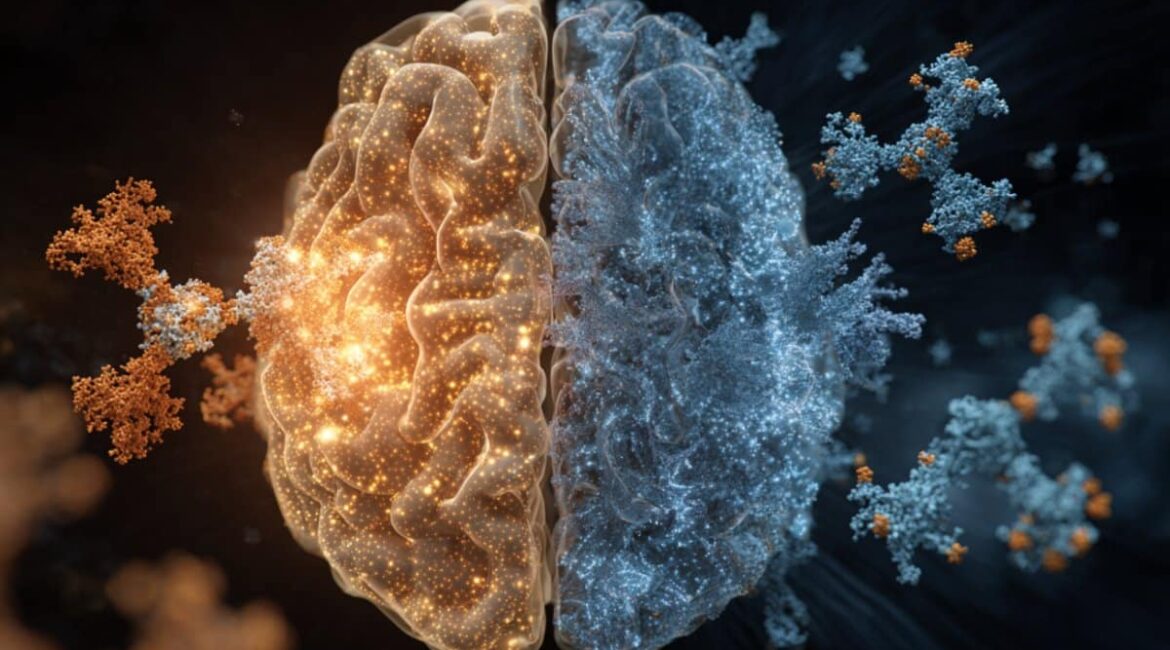
Image: The image is credited to Neuroscience News
Open access to original research
Fernando Gonzalez-Ortiz and colleagues ‘” The potential dual role of tau phosphorylation: Plasma p-tau217 in newborns and Alzheimer’s disease.” Brain Communications
Abstract
The potential dual effects of tau phosphorylation: Alzheimer’s disease and newborn plasma p-tau217
Important aspects of brain pathology and physiology are involved in tau phosphorylation.
It supports microtubule dynamics and neuroplasticity during the development of the foetus, while Alzheimer’s disease ( AD ) causes pathological tau aggregation and tangle formation.
In this multicentre study, we measured plasma phosphorylated-tau217 in healthy newborns, premature infants, patients with AD, and healthy controls across all age groups ( nbsp, = 462 ).
Newborns had significantly higher plasma phosphorylated-tau217 levels than healthy adults of any age group, and they even had levels that exceeded those seen in AD patients. Plasma phosphorylated-tau217 levels in newborns are inversely related to perinatal factors like gestational age.
Preterm infants ‘ serum phosphorylated-tau217 levels declined over the first few months of life, nearly reaching levels seen in young adults, according to a longitudinal analysis of this population.
In contrast, older people had an association with AD pathology because of higher plasma phosphorylated-tau217 levels.
Our findings confirm the crucial role that tau phosphorylation plays in early brain development. However, tau phosphorylation transforms into a pathological process in AD.
The presence of high blood-based phosphorylated tau217 levels during the first few years of life may point to novel regulatory mechanisms that prevent tau aggregation.
The shared mechanisms of tau phosphorylation in newborns and AD need to be investigated further.