Summary: People who have experienced depression may keep a greater sense of consequence and negative feedback perhaps after symptoms subside. A new study found that those with relapsed depression retain the brain’s habenula, which is crucial for processing aversive signals, especially when they are anticipating annoying outcomes.
Additionally, these individuals showed less connection between the habenula and the prize regions, which suggests that stress-related responses are still largely unregulated. The results may provide a better way to identify those who are still at risk and explain why up to 80 % of persons return within five years.
Important Information
- Habenula Hyperactivity: Reported depression sufferers displayed increased habenula engagement as punishment anticipation increased.
- Reduced Reward Circuitry: Connectivity between the reward-related and habenula methods was reduced.
- Return Risk Insight: These frequent changes may inform the development of novel preventive measures to explain high relapse rates.
Origin: Authorship
Researchers have discovered that people who previously had depression may continue to have heightened sensitivity to bad cues and have difficulties regulating their reactions to potential sentence even after recovery.
The results from the publications by Elsevier, including the New study and in Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, could improve our ability to identify those at risk of relapse and guide the development of more precisely targeted treatments to improve long-term healing and prevent upcoming episodes of depression.
Up to 80 % of people who relapse after five years experience a gain of ailments, which demonstrates that treatment does not always guarantee long-lasting endurance. This is a hallmark of despair. A better understanding of the underlying methods that increase a person’s risk of relapse is required to improve protection.
The high return rates observed in melancholy suggest that there must be continuous processes in the brain that make people prone to coming episodes, yet after symptoms have improved, according to lead investigator Henricus G. Ruhé, MD, PhD, from the Department of Psychiatry and Donders Institute for Brain-Cognition and Behavior, Nijmegen, Netherlands.  ,
” People with depression frequently remain vulnerable to punishment, even after recovery,” according to previous studies. This led us to concentrate on aversive learning, a type of Pavlovian traditional heating in which a person learns to avoid a signal or behavior by afflicting it with an unpleasant results.
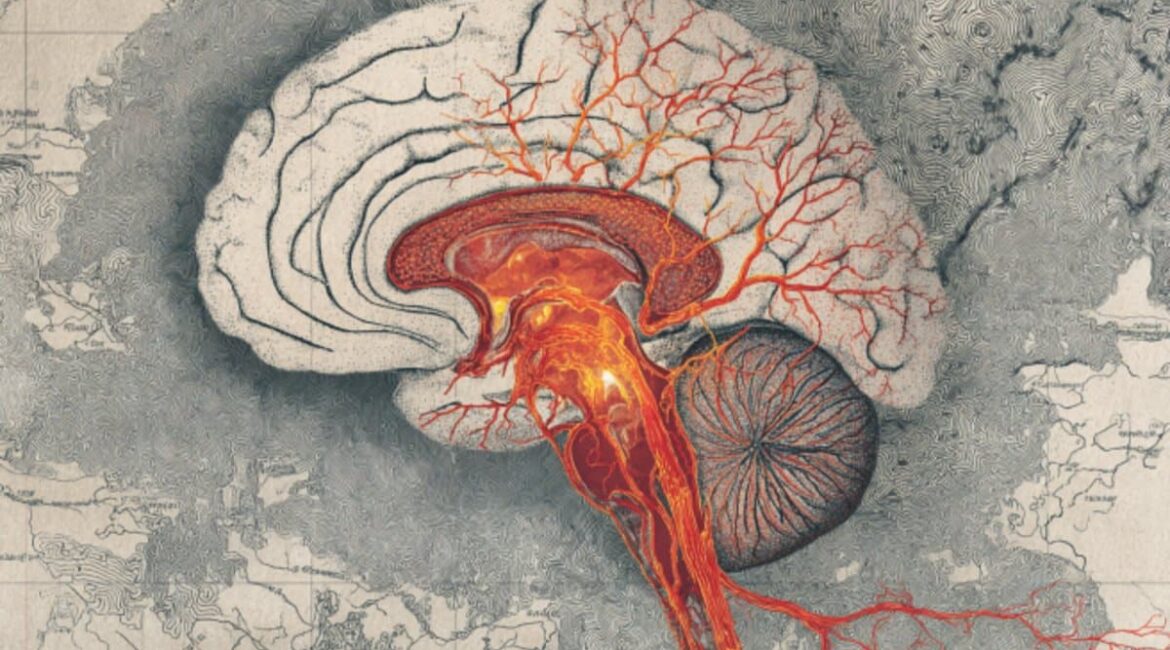
We focused on the habenula, a small area of the brain responsible for processing unfavorable suggestions. We were curious to know whether certain abnormalities in this program persist even after a person recovers from depressive signs.
In this study, researchers used functional MRI ( fMRI ) to measure brain activity in 36 patients with recurrent depression and 27 healthy controls to study aversive learning task. Participants learned connections between a photo and an uncomfortable, harsh taste while undergoing the ultrasound scan.
Imaging revealed proof that relapsed depressed patients had increased habenula activity, especially during the desire of abuse, as well as decreased connectivity between the habenula and the dorsal tegmental area, an essential midbrain nucleus that produces the reward-related neurotransmitter dopamine and an area thought to be regulated by habenula activity.
Even after symptoms have subsided, these designs suggest a heightened responsiveness to bad cues and a lessening ability to regulate responses to possible punishment.
Cameron S. Carter, MD, University of California Irvine, editor-in-chief of Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, concludes,” While little is known about how depression affects mental performance during active condition, we have little understanding of whether these changes persist after recovery.
This study highlights that even when people no longer exhibit obvious signs of depression, they may still have heightened sensitivity to negative signals, which could increase the risk of relapse.
Understanding these persistent effects could help identify at-risk individuals and create more targeted interventions to promote long-term recovery and stop future depressive episodes.
About this news about neuroscience and depression
Author: Eileen Leahy
Source: Elsevier
Contact: Eileen Leahy – Elsevier
Image: The image is credited to Neuroscience News
Open access to original research.
Henricus G. Ruhé and colleagues wrote the paper titled” Aberrant Aversive Learning Signals in Remitted Patients with Recurrent Depression.” Cognitive Neuroscience and Neuroimaging are two branches of biological psychology.
Abstract
Aberrant Aversive Learning Signals in Remitted Patients with Recurrent Depression
Background
One of the main characteristics of major depressive disorder is hypersensitivity to punishment. It is thought that the idea of hypersensitivity to punishment comes from aversive learning.
The habenula is one of the most important components of aversive learning. Although there is strong evidence for dysfunctional aversive learning in depressed patients, whether this dysfunction and its neural correlates persist during symptomatic remission of depression is largely unexplored.
Methods
Within a computational modeling framework, we evaluated functional MRI data from 36 medication-free remitted patients with recurrent major depressive disorder ( MDD ) and 27 healthy control subjects who participated in a Pavlovian classical conditioning task.
Additionally, generalized psychophysiological interaction analyses were carried out to assess the temporal difference signal’s functional connectivity using the habenula as an priori, priori, region of interest.
Results
Patients ‘ bilateral habenula showed significantly more temporal difference-related aversive learning activation than healthy controls. This activation was related to the residual symptoms in the relapsed MDD patient. In addition, patients showed less functional connectivity between the ventral tegmental area and the habenula compared to controls.
Conclusions
In relapsed MDD patients, the increased habenula activity and decreased functional habenula-ventral tegmental area connectivity are a result of aversive environmental sensitivity and/or inability to control the effects of aversive behavior and punishment.
Trial Registration
NTR3768