Summary: Researchers have developed a promising CAR-T body treatments targeting glioblastoma, the most violent brain tumor. Potentially overcoming the limitations of conventional treatments, the treatment uses genetically modified T cell to target a particular symbol on tumor cells.
Importantly, these CAR-T tissue also show an ability to fight cyst cells lacking the symbol, suggesting a witness effect. Early clinical studies in animals demonstrate that this method successfully controls tumor growth with little contamination, setting the stage for human clinical trials.
Important Information:
- CAR-T treatment targets glioblastoma, a very violent brain tumor.
- The treatment shows a “bystander result”, attacking tumor tissues without the destination marker.
- In mouse types, it extended life without considerable toxicity, promising safer remedies.
Origin: University of Geneva
The most prevalent and aggressive primary brain tumor is glioblastoma, which has an average survival time of less than two years after diagnosis and is ineffective in comparison to other key brain tumors. Treatments have recently given sufferers renewed wish, albeit with comparatively minor accomplishment.
A collaboration between the University of Geneva ( UNIGE ) and Geneva University Hospitals ( HUG) managed to identify a particular marker on the surface of tumour cells and create immune cells carrying an antibody to kill them.
However, these cells, called CAR-T cells, appear to be capable of targeting damaged cells in the tissue that do not have this protein, while sparing healthier cells.
These findings, published in the journal , Cancer Immunology Research, are a first step towards the development of clinical studies with individual patients.
Glioblastomas have a variety of genetic characteristics that make them particularly challenging to treat. They escape conventional treatments and recur frequently because they can create a environment that restricts the immune system’s ability to attack.
Denis Migliorini, assistant professor in the Department of Medicine at the UNIGE Faculty of Medicine, member of the Translational Research Centre in Onco-Haematology ( CRTOH) and visiting physician in charge of the HUG Neuro-oncology Unit, is an expert in CAR-T cells ( for chimeric antigen receptors T cells ).
This immunotherapy involves taking defense T cells from patients, genetically altering them in the laboratory to render them show antibodies capable of detecting elements particular to tumor cells, and then reinjecting them so that they can precisely target the tumour.
According to Denis Migliorini,” for several years we have been trying to identify the peptide signs expressed by glioblastoma cells.”
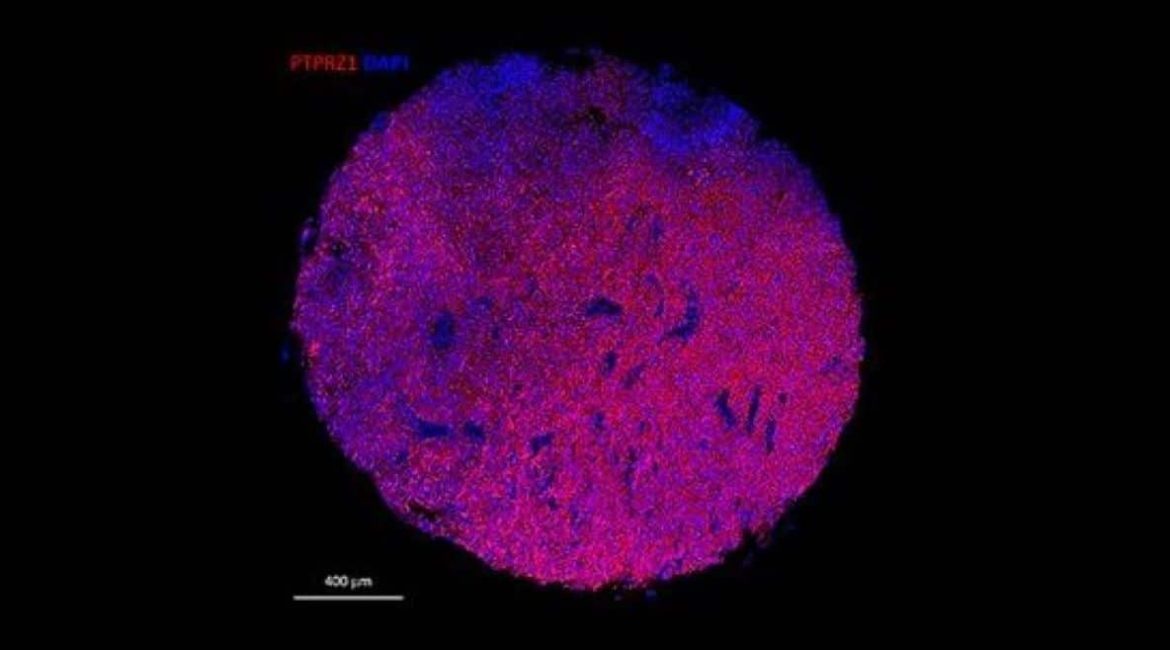
‘ ‘ One of these signs, PTPRZ1, proved especially important: we were able to make CAR-T tissues carrying antibodies targeting PTPRZ1. This is a primary step toward the treatment of malignant cancer with CAR-T cells.
mRNA to make a personalized cell ,
The majority of CAR-T cells are created using popular vectors, a method that has proved effective in treating some conditions but is not particularly effective in the brain.
‘ ‘ Truly, they persist for a very long time in the context body tumors. The mind is a delicate instrument, and this resilience can create a risk of toxicity,” explains Darel Martinez Bedoya, a post-doctoral fellow in Denis Migliorini’s laboratory and primary author of this research.
So, the researchers included the messenger RNA needed to encode the desired antibodies in the T cells. Finally, in order to create the appropriate protein, the biological machinery must produce the necessary protein to construct the receptor that may appear on the T-cell surface and identify the tumor target.
” This method has a number of advantages: CAR-Ts offer a adaptable system, allowing various adaptations according to the specificities and development of the tumour,” explains Darel Martinez Bedoya.
Performance and safety ,
The Geneva group first tested CAR-Ts in vitro on good and tumour cells to confirm that they only attack tumour tissue.
‘ ‘ To our surprise, not merely did CAR-Ts no attack good cells, but they were also ready, by bystander effect, of identifying and fighting tumour  , cells not expressing the PTPRZ1 marker,’ ‘ Denis Migliorini is happy to review.
When co-cultured with target positive tumour cells, CAR-Ts are probably capable of secreting pro-inflammatory molecules that are capable of eradicating tumour cells even in the absence of the original marker. ‘
The treatment was tested in vivo in mouse models of human glioblastoma during the second stage. Tumour growth was controlled, prolonging the lives of the mice remarkably well without , signs of toxicity.
We can use fewer cells and significantly reduce the risk of peripheral toxicity by administering CAR-Ts intratumourally in the CNS.  , With this data and other unpublished yet, all lights are green to now envisage a first clinical trial in humans,’ ‘ the scientists conclude.
About this research in glioblastoma brain cancer
Author: Antoine Guenot
Source: University of Geneva
Contact: Antoine Guenot – University of Geneva
Image: The image is credited to Neuroscience News
Original Research: Closed access.
By Denis Migliorini et al.,” PTPRZ1-targeting RNA CAR T cells exert bystander antitumor activity in glioblastoma.” Cancer Immunology Research
Abstract
PTPRZ1-targeting RNA CAR T cells exert antigen-specific and bystander antitumor activity in glioblastoma
The high level of success of the chimeric antigen receptor ( CAR ) T-cell therapy for B-cell malignancies has led to its application to solid tumors.
In the case of glioblastoma ( GBM ), clinical trials have shown modest efficacy, but efforts to develop more effective anti-GBM CAR T cells are ongoing. In this study, we selected PTPRZ1 as a target for GBM treatment.
In an RNA format, we produced second generation CAR T cells from a human phage display library, which contained six anti-human PTPRZ1 scFv.
Patient-derived GBM PTPRZ1-knock-in cell lines were used to determine the CAR construct ( 471_28z ), which consistently displayed high CAR expression while exhibiting high cytotoxicity.
CAR T cells incorporating 471_28z were able to release IFN-γ, IL-2, TNF-α, Granzyme B, IL-17A, IL-6, and soluble FasL, and displayed low tonic signaling. Additionally, they maintained an effector memory phenotype after in vitro killing.
In addition, 471_28z CAR T cells displayed strong bystander killing against PTPRZ1-negative cell lines after pre-activation by PTPRZ1-positive tumor cells but did not kill antigen-negative non-tumor cells.
A single dose of anti-PTPRZ1 CAR T cells significantly delayed tumor growth in an orthotopic xenograft tumor model using NSG mice.
Taken together, these results validate PTPRZ1 as a GBM target and prompt the clinical translation of anti-PTPRZ1 CAR T cells.